For the first time, researchers have shown what happens to the brain when a person receives their first round of repetitive transcranial magnetic stimulation (rTMS) to treat their depression. The results were published today in the American Journal of Psychiatry.
rTMS is a depression treatment typically used when other approaches — such as medications — haven’t been effective for a patient. It is estimated that approximately 40 per cent of people with major depression do not respond to antidepressants.
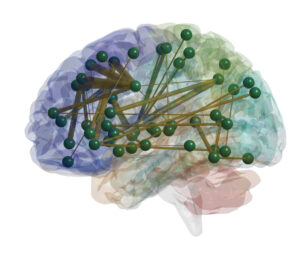
Different regions of the brain are activated during rTMS treatment, including regions that manage emotional responses, memory and motor control.
During an rTMS session, a device containing an electromagnetic coil is placed against a patient’s scalp. The device then painlessly delivers a magnetic pulse that stimulates nerve cells in a region of the brain involved in mood control — called the dorsolateral pre-frontal cortex.
Although proven to be effective, the mechanisms behind how rTMS affects the brain have not been well understood.
“When we first started this research back in 2014, the question we were asking was very simple: we wanted to know what happens to the brain when rTMS treatment is being delivered,” says Dr. Fidel Vila-Rodriguez, an Assistant Professor in UBC’s Department of Psychiatry and researcher at the Djavad Mowafaghian Centre for Brain Health (DMCBH).
Vila-Rodriguez set out to answer this question. His team delivered one round of rTMS to people diagnosed with depression while they were inside a magnetic resonance imaging (MRI) scanner. Since the MRI can measure brain activity, the researchers were able to see in real time what changes were happening in the brain as rTMS was being delivered.

Dr. Vila-Rodriguez demonstrates rTMS testing in the MRI machine.
The team found that by stimulating a part of the brain called the dorsolateral pre-frontal cortex with rTMS, several other regions of the brain were activated. These other regions are involved in multiple functions — from managing emotional responses to memory and motor control.
After receiving their first rTMS session in the scanner, participants underwent another four weeks of rTMS treatment and the team assessed whether the activated regions were associated with participants having fewer symptoms of depression when their treatment ended.
“We found that regions of the brain that were activated during the concurrent rTMS-fMRI were significantly related to good outcomes,” says Vila-Rodriguez.
With this new map of how rTMS stimulates different areas of the brain, Vila-Rodriguez hopes the findings could be used to determine how well a patient is responding to rTMS treatments.
“By demonstrating this principle and identifying regions of the brain that are activated by rTMS, we can now try to understand whether this pattern can be used as a biomarker, or if this treatment can be helpful in other neuropsychiatric disorders.”
This research was a collaborative effort across the Centre for Brain Health, including DMCBH researchers Dr. Sophia Frangou, Dr. Rebecca Todd, and Dr. Erin MacMillan, as well as members of the UBC MRI Research Centre including Laura Barlow.
Vila-Rodriguez has received a grant from the Canadian Institutes of Health Research to study whether this pattern of activation can be detected by changes in heart rate. He also received funding through the Djavad Mowafaghian Centre for Brain Health Alzheimer’s Disease Research Competition to look at rTMS as a way to enhance memory in patients who are showing early signs of Alzheimer’s disease.
He hopes this type of research will encourage the government to offer rTMS across the country. Despite being approved by Health Canada 20 years ago, rTMS is still not widely available. In BC, there are some private clinics that offer it, but it is still not covered by the provincial health plan.


