In a new paper recently published in the journal Stem Cell Reports, UBC researchers found that familial Alzheimer disease can be transferred via bone marrow transplant. When the team transplanted bone marrow stem cells from mice carrying a hereditary version of Alzheimer disease into normal lab mice, the recipients developed Alzheimer disease—and at an accelerated rate.
The study highlights the role of amyloid that originates outside of the brain in the development of Alzheimer disease, which changes the paradigm of Alzheimer’s from being a disease that is exclusively produced in the brain to a more systemic disease. Based on their findings, the researchers note that donors of blood, tissue, organ and stem cells should be screened for Alzheimer disease to prevent its inadvertent transfer during blood product transfusions and cellular therapies.
“This supports the idea that Alzheimer’s is a systemic disease where amyloids that are expressed outside of the brain contribute to central nervous system pathology,” says senior author Dr. Wilfred Jefferies, an immunologist in UBC’s Department of Medical Genetics and a DMCBH member. “As we continue to explore this mechanism, Alzheimer disease may be the tip of the iceberg and we need to have far better controls and screening of the donors used in blood, organ and tissue transplants as well as in the transfers of human derived stem cells or blood products.”
To test whether a peripheral source of amyloid could contribute to the development of Alzheimer’s in the brain, the researchers transplanted bone marrow containing stem cells from mice carrying a familial version of the disease—a variant of the human amyloid precursor protein (APP) gene, which, when cleaved, misfolded and aggregated, forms the amyloid plaques that are a hallmark of Alzheimer disease. They performed transplants into two different strains of recipient mice: APP-knockout mice that lacked an APP gene altogether, and mice that carried a normal APP gene.
In this model of heritable Alzheimer disease, mice usually begin developing plaques at 9 to 10 months of age, and behavioural signs of cognitive decline begin to appear at 11 to 12 months of age. Surprisingly, the transplant recipients began showing symptoms of cognitive decline much earlier—at 6 months post-transplant for the APP-knockout mice and at 9 months for the “normal” mice.
“The fact that we could see significant behavioural differences and cognitive decline in the APP-knockouts at 6 months was surprising but also intriguing because it just showed the appearance of the disease that was being accelerated after being transferred,” says first author Dr. Chaahat Singh, a postdoctoral fellow in the Jefferies lab.
In mice, signs of cognitive decline present as an absence of normal fear and a loss of short and long-term memory. Both groups of recipient mice also showed clear molecular and cellular hallmarks of Alzheimer disease, including leaky blood-brain barriers and buildup of amyloid in the brain.
Observing the transfer of disease in APP-knockout mice that lacked an APP gene altogether, the team concluded that the mutated gene in the donor cells can cause the disease and observing that recipient animals that carried a normal APP gene are susceptible to the disease suggests that the disease can be transferred to healthy individuals.
Because the transplanted stem cells were hematopoietic cells, meaning that they could develop into blood and immune cells but not neurons, the researchers’ demonstration of amyloid in the brains of APP knockout mice shows definitively that Alzheimer disease can result from amyloid that is produced outside of the central nervous system.
Finally, the source of the disease in mice is a human APP gene, demonstrating the mutated human gene can transfer the disease in a different species.
In future studies, the researchers plan to test whether transplanting tissues from normal mice to mice with familial Alzheimer’s could mitigate the disease, test whether the disease is also transferable via other types of transplants or transfusions and expand the investigation of the transfer of disease between species.
“In this study, we examined bone marrow and stem cells transplantation,” says Dr. Jefferies. “However, next it will be important to examine if inadvertent transmission of disease takes place during the application of other forms of cellular therapies, as well as to directly examine the transfer of disease from contaminated sources, independent from cellular mechanisms.”
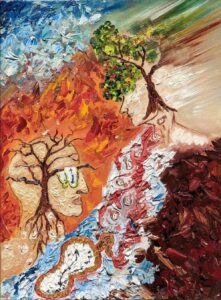
Pictured here is original artwork created by Dr. Singh, which was featured on the cover of the latest issue of Stem Cell Reports. She describes the inspiration behind the painting:
“Inspired by Salvador Dali’s painting “The Persistence of Memory” the image depicts the melting clocks as stem cells being transferred from an Alzheimer’s patient to a healthy individual where the vibrant foliage turns into a blur representing Iatrogenic cognitive decline. The melting clocks going upstream portray the distortion of time in AD patients. At a second glance, the big clock shows the numbers stacked to one side, a test used to screen for early dementia.
In the surrealist tapestry of time, where memories may drip and melt like Dali’s clocks, the persistent canvas of the mind clings to the fragmented droplets, painting a mosaic of recollections even in the face of elusive amnesia.”
A version of this story was originally published on the EurekAlert! website.


