Parkinson disease not only affects movement but also profoundly impacts emotions and cognitive functions, which poses significant challenges for treatment. While therapies exist for motor symptoms, addressing emotional and cognitive issues, known as non-motor symptoms, remains elusive and greatly affect patients’ quality of life.
Dr. Stefan Lang is a DMCBH member and Clinical Assistant Professor in the Division of Neurosurgery at UBC whose research focuses on deep brain stimulation (DBS), a technique involving the implantation of electrodes deep within the brain to treat dysfunctional circuits. While DBS effectively manages motor symptoms, its efficacy in alleviating non-motor issues varies.
“In our latest research study, we are using state-of-the-art neuroimaging analysis combined with detailed clinical data collection to understand some of this variability,” explains Dr. Lang. “We hypothesize that engagement of specific brain networks, influenced by the exact position of the electrode deep in the brain, can help us better understand how DBS impacts non-motor symptoms.”
Expanding the use of deep brain stimulation
Clinical experience has shown that DBS is very effective in treating movement disorders such as Parkinson disease, dystonia and essential tremor. There is also evidence that it can help with some epilepsy and psychiatric conditions. In general, these diseases all have a well-defined pathological neural circuit.
Recently, researchers have also been interested in assessing the effects of using DBS in treating Alzheimer disease by targeting a part of the brain called the fornix, which plays a key role in cognition and memory recall. While this research is still ongoing, these new applications of DBS are promising and will continue to expand as neuroscientists gain a better understanding of dysfunctional brain circuits in various neurodegenerative diseases.
Since new DBS devices are approved to be safely used in 3T MRI machines, Dr. Lang and his team are hoping to take advantage of this in future research studies by performing simultaneous DBS and functional magnetic resonance imaging (fMRI).
“From a basic science perspective, DBS/fMRI is a powerful tool for simultaneously modulating and observing neural activity,” he says. “From a clinical perspective, DBS/fMRI has identified network biomarkers of optimal motor outcomes, which can be used to confirm circuit engagement and refine DBS programming strategies.”
Dr. Lang notes it is important to understand that DBS is a symptomatic treatment and does not slow down or reverse the neurodegenerative process. However, a better understanding of how DBS modulates distributed brain networks will help optimize the treatment and offer new hope for both physical and cognitive challenges faced by Parkinson disease patients.
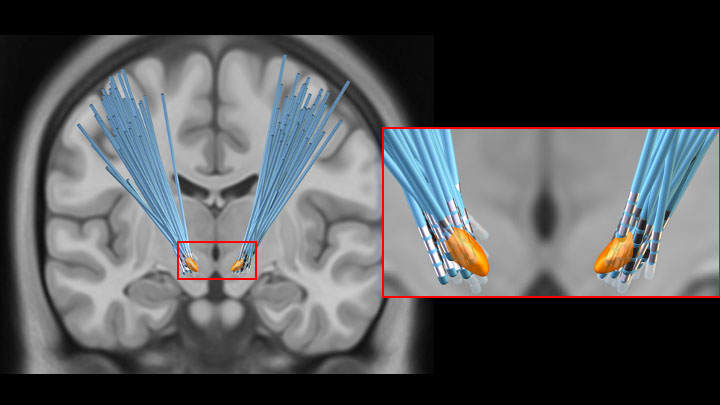
This image shows reconstructed electrodes for 65 patients with STN DBS. Small variations in electrode position can influence clinical outcomes through differential network modulation.
Combining research and clinical work
Dr. Lang was originally interested in studying the “big problems” of neuroscience, such as consciousness. Over time, he developed a more humanitarian perspective and decided to combine his scientific interests with a more practical application.
“I was drawn to neurosurgery – specifically functional neurosurgery – which is an established, but rapidly evolving surgical specialty that lies at the intersection of neurosurgery, neurology and psychiatry,” says Dr. Lang. “In this capacity, I have the immense privilege of directly helping patients on a day-to-day basis, with surgeries such as DBS, while also having the unique opportunity to study the human brain along the way.”
Recently, he was selected as one of the recipients of Vancouver Coastal Health Research Institute’s 2024 Mentored Clinician Scientist awards, which will help expand his research capacity. This is crucial as he builds up his research program and forges new collaborations with other members of the DMCBH.
One of the other projects that Dr. Lang is also leading involves the collection of advanced neuroimaging and cognitive outcomes from brain tumour patients before and after surgical resection.
In the future, another area that Dr. Lang hopes to study is intracranial neurophysiology.
“All my patients are awake while I perform single-cell recording for the purposes of accurately placing the DBS electrodes,” he explains. “These patients are often happy to participate in brief cognitive tasks during this time, so we are beginning to explore this as a unique opportunity for data collection.”
Since his PhD work focused on non-invasive brain stimulation techniques, he is also interested in exploring various incisionless therapies, especially focused ultrasound. Developing non-invasive therapies would expand available treatment options that would greatly benefit patients with various brain disorders.


