Imagine if you could get your brain scanned at the doctor’s office without having to book a separate appointment. This could soon be a reality as Dr. Shannon Kolind and her research team are working to bring the world’s first commercial point-of-care magnetic resonance imaging (MRI) scanner into the clinics at the Djavad Mowafaghian Centre for Brain Health (DMCBH), and eventually out into the community.
Dr. Kolind, an associate professor in the Faculty of Medicine and researcher at the DMCBH, is the UBC lead of the UNITY (Ultra-Low field Neuroimaging In The Young) project, funded by the Bill and Melinda Gates Foundation. The project aims to explore how Hyperfine’s portable MRI can be used in pediatric populations of low- and middle-income countries, with a particular interest in the effect of malnutrition on myelin in brain development.
With funding from Brain Canada and Michael Smith Health Research BC, Dr. Kolind is also looking at new MRI applications in multiple sclerosis (MS). This disease is caused by inflammation of the nervous system and results in demyelination, the process by which the myelin sheath (the protective layer around nerves) is destroyed.
There are three main MRI techniques that Dr. Kolind and her team are working on that examine different ways to measure myelin changes in pediatric and MS populations. These techniques can help monitor disease progression, detect new brain lesions and see if myelin can be repaired.
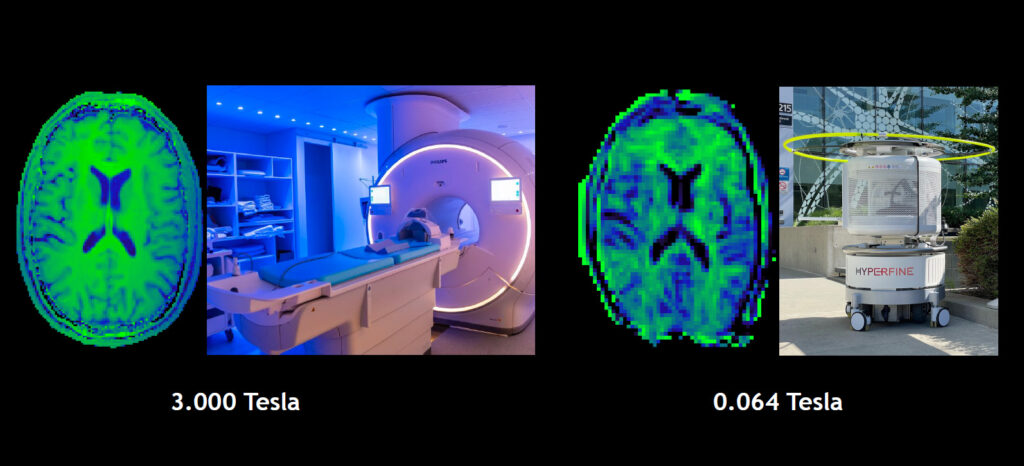
Magnetization transfer imaging comparison between traditional 3T MRI and Hyperfine point-of-care scanner.
The first is magnetization transfer imaging, an MRI technique that examines the interaction between macromolecules and water. This technique was developed in collaboration with Hyperfine over the last year and was recently tested for people living with MS in January.
“A major source of macromolecules in the brain’s white matter is myelin, so if we see a big effect in the transfer of energy that means a lot of myelin is present and if we see a small effect, then there is less myelin present,” Dr. Kolind explains. “This is novel at low-field and has never been done before on this type of point-of-care scanner.”
The second technique is T2 mapping, which provides information about the nature of the environment that water is in. Because quantitative intrinsic values can be mapped, this makes it more reliable and easier to track changes that occur over time.
This process can be taken one step further with myelin water imaging, which was pioneered by Dr. Alex MacKay at UBC. Using this technique, researchers can look specifically at water associated with myelin and get a very specific measurement of myelin. In particular, PhD student Adam Dvorak has found benefits of working with a low-field scanner. Because there is less heating, data can be collected at a higher rate compared to a high-field scanner.
The third technique is specific to MS, using a type of image called FLAIR (fluid-attenuated inversion recovery) to look at brain lesions. UBC is the first site that has been able to optimize FLAIR scans based on images from people with MS, as this technique has not previously been fine-tuned to look specifically at MS lesions with this point-of-care scanner.
Based on the team’s knowledge of MS, graduate students Sharada Balaji and Neale Wiley have been working on adjusting parameters in the MRI sequences to get rid of some of the artefacts in the images and altering the resolution so that lesions are more visible. Dr. Anthony Traboulsee has also played an important role in recruiting participants and providing input on the clinical side of things.
“It’s been a collaborative effort between our research team and Hyperfine,” says Dr. Kolind. “They’ve been helping us understand how the sequences are working and providing access to the code, and in turn we’ve provided them with data from our scans so that they can improve their software.”
Using machine learning to create sharper images
With today’s technology, smartphones use machine learning to automatically adjust camera lighting and focus, and can take multiple photos at different exposures to blend them together in post-processing to create one high-quality photo. Similarly, Hyperfine’s portable MRI is able to use artificial intelligence (AI) to make adjustments during the image reconstruction process to improve the quality of scans by reducing image blurring and noise.
“With a lot of the tricks that we’re developing, like machine learning and different algorithms, we only need to collect a fraction of the data but can still reconstruct complete images,” Dr. Kolind explains. “We can basically make tweaks and fill in the gaps because of the patterns we see in the data, which speeds things up substantially.”
As Hyperfine rolls out new software updates, the image quality of scans will continue to improve. The more data that gets collected over time, the easier it will be for researchers to refine machine learning models to more efficiently and accurately reconstruct images.
“Generally, we turn off the machine learning feature and look at the raw data because we want to understand all the steps involved behind the scenes, but once we understand the process, we can see if AI can help us get the same result,” says Dr. Kolind. “However, these tools are all being rigorously tested before use in clinical settings, to make sure we’re not missing anything that could lead to a misdiagnosis.”
Exploring other uses of portable MRI
Dr. Kolind and her team are working in collaboration with other clinicians at the DMCBH to test additional applications for this scanner. For example, Dr. Fidel Vila-Rodriguez is looking to utilize ultra-low field MRI in transcranial magnetic stimulation (TMS) to treat depression. Usually, it takes some experimenting to figure out the proper spot to apply TMS treatment. It’s been shown that it can be a lot more effective to get precise positioning by using MRI, but to do that in a clinical setting is prohibitively expensive. If the portable MRI can be used to obtain images that are optimized for TMS, that would be much more cost-effective and greatly benefit people who suffer from depression.
In general, the portable MRI is much cheaper to operate than a traditional MRI scanner, as it can be plugged into a regular wall outlet and uses very little electricity – less than the average blender! It is also easy to transport and does not require highly trained personnel to operate.
From a patient’s point of view, they are a lot more comfortable and do not feel as claustrophobic because only their head is placed inside the machine. Patients are also not in an isolated room so staff and even family members can be close by throughout the scan, which opens up many possibilities for use in pediatric settings involving young children.
Ideally, the portable MRI will become a permanent resource in the Charles E. Fipke Integrated Neuroimaging Suite at the Djavad Mowafaghian Centre for Brain Health. With its close proximity to the clinics and traditional 3T MRI scanner, it will be a valuable tool in providing clinical care.
“We would also like to purchase another scanner for research purposes, to develop more utility and advanced MRI techniques,” says Dr. Kolind. “This would allow collaborations with more research groups and lead to more clinical applications.”
Another long-term goal is to have a mobile unit that could be taken out to the community, especially rural locations. With the lessons learned from the UNITY project, Dr. Kolind and her team would plan to make further refinements and improvements before it is used with the general population.
“We want to ensure the scanner can meet the needs of the community so it’s not adding more burden to the healthcare system but actually taking some of the pressure off,” says Dr. Kolind. “By integrating it with existing workflows, this can empower communities that don’t currently have adequate resources and could help reduce the pressure on our existing medical imaging infrastructure.”



